Abstract
The aim of this study was to compare in vivo effects of single and repetitive doses of betamethasone (BETA) and dexamethasone (DEX) administered to pregnant mice on lung maturation and lung, liver, and body weights (LLBW) of their pups. One hundred and eighty gravid Swiss albino mice were randomly assigned to 1 of 6 groups (n = 30) and administered either BETA, DEX, or saline as a single dose at 14 d gestation or repetitive doses twice daily at 14 and 15 d gestation. All the study groups were then divided into three sets (n = 10). The mice in the second sets were redivided into three subsets randomly (including four, three, and three mice). All gestations in the first sets were terminated at 16.5 d gestation to observe the neonatal breathing pattern (scale to 0–5; 5 is unlabored breathing) of male and female pups whereas other sets had normal delivery. The pups in first, second, and third sets were killed for evaluation in the first set after the evaluation of breathing pattern, in the subsets of second set on postnatal d 1, 3, and 5, and in the third set on postnatal d 90. We recorded maternal body weights at 0 and 16.5 d gestation, and LLBW, the lung/body weight ratio of pups, sex, and the amount of live and dead births per litter. Pups exposed to BETA and DEX had significantly lower maternal weight compared with the saline groups. The death litter size was significantly higher in pups exposed to repetitive doses of DEX than the other treatments. Sex had no significant effect on breathing score and LLBW. Pups exposed to repetitive doses of BETA and DEX presented a higher breathing score than the other groups. The breathing score was significantly higher with BETA than DEX after their repetitive use. The LLBW were significantly less in the treatment groups, especially in the group exposed to repetitive doses of DEX. In conclusion, repetitive doses of BETA and DEX lead to increased fetal lung maturation, but this may be at the expense of fetal and neonatal growth. DEX is less potent in accelerating lung maturation than BETA but it causes more reduction in fetal and neonatal growth.
Similar content being viewed by others
Main
Prenatal GC therapy is routinely used to improve infant outcome after preterm birth, although a number of questions regarding its clinical use could not be answered with available experimental and clinical literature (1). Crowley et al. (2) indicate that prenatal GC therapy is optimally effective if the treatment-to-delivery interval is 24 h to 7 d (3). Many fetuses at risk of preterm delivery do not deliver within 7 d of initial GC treatment. As a result, obstetricians are frequently administering repetitive courses of maternal GC therapy at 7-d intervals to achieve a maximal fetal response in pregnancies with early preterm labor (<32 wk) (4, 5), although there are no randomized controlled trial data to support this practice.
Despite the widespread use of antenatal corticosteroid therapy in obstetric practice, little is known about the effects of synthetic GC on the fetal tissues. Some effects of prenatal GC use on lung structure (6), somatic growth, brain maturation (7), and adrenocorticoid function (8) after repeated GC treatments can persist until delivery at term. At this time, having overcome the immediate issue of LM and survivability, the improvement of treatment protocols continues. Therefore, questions currently being asked are directed at the side effects from such treatment, in particular, from repeated dosing, which have already stated that it has not been sufficiently addressed. Studies from the 1970s demonstrated decreased fetal growth and weight in rats (9, 10), rabbits (11), and humans (12) after antenatal corticosteroid use. However, few studies compared the effect of both BETA and DEX on fetal LLBW (13).
The aim of this study was to investigate in vivo effects of single or repetitive doses of BETA and DEX administered to pregnant mice near the end of the last third of the gestation period on fetal LM and LLBW of their pups.
MATERIALS AND METHODS
Animals.
All procedures were approved and performed under the guidelines of the Animal Care and Use Committee of Cumhuriyet University School of Medicine. Experiments were carried out on Swiss albino female mice (26–33 g body weight) maintained in individual cages under controlled temperature (21–23°C), a relative humidity of 60–65%, and day light, and fed ad libitum. Each mouse was assigned an identification pairing number before mating. Attempts at conception were undertaken for up to 5 consecutive days (one estrus cycle). The timed conception was identified as gestational d 0 by the presence of a copulatory plug during a 2-h exposure (0900–1100 h) with the male. The pregnant females were then housed individually throughout gestation.
At 13 d gestation, the gravid mice (n = 180) were randomly assigned to one of the six treatment groups: SB, RB, SD, RD, SS, and RS groups. Each group was then divided into three sets of 10 mice randomly. We recorded body weights of all mice at 0 and 16.5 d gestation. Mice with a litter size smaller than two were excluded.
Fetal treatments.
We used mouse model of Stewart et al.(14). to investigate the effect of BETA and DEX on LM and LLBW of mouse pups. Doses of BETA and DEX from previous studies of Stewart et al. (14) and Christiensen et al. (15), respectively, were given as single or repetitive doses of BETA or DEX. We used BETA (Celestone Chronodose; Eczacibasi Pharmaceuticals Co., Istanbul, Turkey) and DEX (Deksamet; Biosel Pharmaceuticals Co., Istanbul, Turkey) formulations, used in animal and human investigations, composed of an equivalent molar weight mixture of the sodium phosphate and acetate forms (16, 17). The 6 mg/mL solution of BETA and 8 mg/mL solution of DEX were diluted with 0.9% sodium chloride solution to prepare a 0.1-mg dose in 0.25 mL. These doses of BETA and DEX have been shown to accelerate fetal lung maturity without impairing fetal survival or weight gain (15) are the most common formulations used clinically.
Each mouse received either saline (0.9% sodium chloride) or BETA or DEX as a 0.25-mL dose drawn into 1-mL syringes. A 25-gauge needle was used for subcutaneous injection into the nuchal fold. We administered single dose of BETA, DEX, and saline solution at 0900 h at 14 d gestation in the SB, SD, and SS groups, respectively, and repetitive doses of BETA, DEX, or saline solution twice daily (0900 h/2100 h) at 14 and 15 d gestation in the RB, RD, and RS, respectively.
Postnatal measurements.
In the first set of all the groups, the gravid mice (n = 60) were killed by cervical dislocation at 16.5 d gestation. The pups, removed by immediate hysterotomy, were placed on a filter paper moistened at 37°C. Lung maturity was evaluated with a previously established technique designed to characterize breathing effort by the study of Christensen et al. (15). Each pup's breathing motion was observed for 1 min by the same investigator (T.G.), who was blinded to the treatment. We used a scoring assignment according to the respiratory pattern: 0, no breathing; 1, gasping; 2, gasping/labored breathing; 3, labored breathing; 4, labored breathing/unlabored breathing; 5, unlabored breathing. Gasping was characterized as isolated breathing with the mouth opened and the neck extended. Labored breathing involved abdominal and extremity movement, whereas unlabored breathing required chest motion only. After BS test, the pups of the first set were killed for evaluation.
Beginning at 18.5 d gestation, the gravid mice in the second and third sets were checked twice daily for the presence or absence of any litters and we waited for their delivery in term gestation. The mice in the second set of all the groups were redivided into three subsets randomly (including four, three, and three mice) and we killed their pups for evaluation on postnatal d 1, 3, and 5, respectively. The pups of third set of all the groups were killed for evaluation on postnatal d 90. The amount of live and dead births per litter, LLBW, the lung/body weight ratio, and the sex of pups were determined at the appropriate time according to the set and subsets of all the groups.
Statistical analysis.
The effect of antenatal treatment on prenatal and postnatal parameters was examined by one- or two-way GLM univariate ANOVA. Where the difference between treatment groups was significant, post hoc pair-wise comparisons between study groups were performed using Tukey HSD multiple comparisons test. With a special feature of this post hoc test, the study groups were classified into homogeneous subsets and these subsets were shown from “a” to “f” letters where appropriate in data presentations. Sex ratio of pups in study groups was compared by χ2 test. Statistical significance was accepted at p < 0.05.
RESULTS
We found no significant difference in maternal weights at 0 d gestation among study groups (Table 1). Although the maternal weight increases during pregnancy, at 16.5 d gestation, mice exposed to BETA and DEX, especially in the RD group, had significantly lower maternal weight compared with the saline groups, respectively (p < 0.05;Table 1). There was no significant difference in the sex ratio and live litter size among the study groups, although the live litter size was lower in RD group (p > 0.05;Table 1). The death litter size of RD group was significantly higher than that of the other groups (p < 0.05;Table 1).
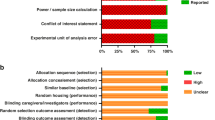
Comparison of the BS of the first set of study groups were performed after pups' sex and study group were given as two factors in the ANOVA test; and the factor of study group only presented significant effect on the BS (p < 0.05;Fig. 1). Later, BS of female and male pups were compared separately. The BS of female and male pups was significantly higher in the four treatment groups compared with the saline groups (p < 0.05). There was significantly higher BS of female and male pups in the repetitive GC-exposed groups than the single GC-exposed groups (p < 0.05). The BS of female and male pups in the SB and RB groups was significantly higher than that of the SD and RD groups, respectively (p < 0.05). In the four treatment groups, the male pups had higher BS than that of the female ones (p > 0.05), but it did not reach statistical significance.
BS of male and female pups delivered at 16.5 d gestation in the first set (n = 10) of the six study groups. There was no significant difference between the male and female sets (p > 0.05); however, the male and female sets were analyzed separately and it was found that there were significant differences among the sets within the female and male groups (p < 0.05). For the female sets, the letters a, b, c, and d were used to designate significance. Sets with the same letter were not significantly different; sets with different letters were significantly different (p < 0.05). Similarly, the letters e, f, g, and h were used for the male group with the same interpretation. Comparison of sets used the Tukey HSD multiple comparison test. Data are presented as mean ± SD.
Figures 2 and 3 illustrate LLBW of female and male pups, respectively, in the first sets and the subsets of the second sets of study groups. Table 2 presents LLBW of female and male pups in the third sets of study groups. Table 3 shows lung/body weight ratio of female and male pups in all the sets of study groups. Although we found no significant difference in these findings with respect to sex, they were usually higher in male pups. These findings generally were significantly lower in SB and SD groups, and RB and RD groups than those of the SS and RS groups, respectively (p < 0.05). When pups exposed to the single and repetitive doses of DEX, these findings usually were significantly lower than those of pups given the single and repetitive doses BETA, respectively (p < 0.05). The LLBW of male pups in RB and RD groups were significantly lower than those of male pups in saline groups at birth (p < 0.05). These reductions was persisted into the young adult period (postnatal d 90); however, this was not shown in the females except in liver weight.
DISCUSSION
This study examined the effects of multiple fetal exposures to BETA and DEX at approximately 75% of gestation on postnatal LM and fetal and neonatal growth in doses determined for simulation of those used clinically for fetal LM. Repetitive exposures to GC, especially BETA, given twice daily at 14 and 15 d gestation improved postnatal LM in prematurely delivered pups at 16.5 d gestation. Repeated doses of GC, especially DEX, decreased maternal body weight measured at 16.5 d gestation and LLBW. Their effect on weight reduction persisted on postnatal d 90. Male pups had increased LM and LLBW than female ones but this difference was not reached statistical significance.
Both BETA and DEX appear to be ideal corticosteroids for enhancing fetal maturation when they are given between 24 and 34 wk gestation. These drugs are similar in structure and function, have an approximate plasma half-life of 3–5 h and long biologic half-life of 36–54 h, and cross the placenta in biologically active forms (18). Both clinical and in vitro evidence suggest that corticosteroid-induced biologic effects on the fetal lung persist up to 7 d after their use (17, 19). Both BETA and DEX cross the placenta and are not inactivated to a major extent by placental enzymes. The only difference between them is the orientation of a methyl group on position 16. Although it is hard to explain that such a small difference between two molecules could have considerable results, the biologic effects of photoisomerization of the bilirubin molecule show how a change in orientation can alter its effects. These drugs modulate the rate of differentiation of numerous fetal organs, including lung studied in detail (20), heart, liver, skin, gut, and kidney (17, 21, 22). There is now growing evidence from a number of studies on different species that fetal exposure to excess GC at critical stages of development also can have lifelong effects on several systems. Antenatal treatment with either BETA or DEX at the recommended doses provides similar physiologic stress level of GC activity in fetal plasma sufficient to provide a near-maximal occupancy of receptors and induction of target proteins.
We found that the lung weight was significantly lower after antenatal exposure to repetitive doses of BETA or DEX rather than their single doses. When comparing the two treatment groups, it was observed that DEX markedly reduced the lung weight more than BETA. The reduced lung/body weight ratios further demonstrate the relative loss of lung tissue mass. This reduced weight, evident in both sexes, was not reversible and persisted in the young adults, although the relative lung/body weight ratios tended to normalize. The reduced lung weight after exposure to the single dose of BETA was reversed in the young adults, but their effect after repetitive use persisted. These findings are in accord with the study of Stewart et al. (14). Willet et al. (23) reported that the most striking effect of antenatal use of BETA was a marked reduction in alveolar number by inhibiting alveolar septation in animals treated at 118 or 119 d gestation when alveolar formation is already underway in fetal sheep. In the study of Corroyer et al. (24), newborn rats were given a 4-d treatment with DEX (0.1–0.01 μg/g body weight DEX sodium phosphate daily on d 1–4), or saline. Morphologically, this treatment caused a significant thinning of the septa and an acceleration of LM on d 4. They suggested that GC may accelerate LM by influencing cell cycle control mechanisms, mainly through impairment of G1 cyclin/CDK complex activation. Although Stewart et al. (19) found no long-term differences beyond the immediate perinatal period in the growth and development of BETA- or placebo-exposed mouse pups, Okajima et al. (25) evaluated the influences of antenatal DEX administration on neonatal lung development in rats. They administered DEX (0.4 mg/kg maternal body weight per day) on the 21st d or on the 20th and 21st d of gestation in Sprague Dawley rats. After natural deliveries, the lungs of the pups 1–60 d of age were obtained and processed for morphometric analysis. They found that both groups presented a lower numerical density of alveoli and a larger mean alveolar radius in 60-d-old pups.
The effect of corticosteroids on the liver weight was similar to that on lungs. In general, DEX caused a greater reduction in liver weight than BETA. Several mechanisms for these reductions have been suggested. This mechanism of growth impairment associated with corticosteroid therapy is thought to be related to reduced biosynthesis of DNA and RNA as well as prolonged inhibition of mitosis and cellular activity (12, 26). This reduced weight also may result, in part, from impaired function of the placenta after treatment, but may also be a direct effect of corticosteroids on fetal tissues (27). A previous study showed that there were no differences between BETA and control group in brain, lung, kidney, and adrenal weights in rhesus monkeys (28). However, the mean liver weight of the BETA-treated fetuses was significantly greater than that of the control group. They suggested that the increased liver weight is caused by an elevation in liver glycogen content, however, the specific mechanism is not known (28). Previous studies in fetal sheep have found fetal growth retardation after BETA treatment at 104 d gestation (68% of gestation) but not after later in gestation (29). Antenatal corticosteroids routinely have caused growth retardation in fetal rodents (30, 31). These species have short gestations and rapid fetal growth, and a single treatment will impact significantly.
We found that the body weight of male pups exposed to the repetitive doses of BETA and DEX was lower than those of male pups administered saline solution. The reduction in body weights persisted into the young adult period (postnatal d 90); however, this was not shown in the females. We speculate that the cause of this reduction may be the androgen hormone. Androgens have been found to delay fetal LM, while stimulating fetal lung growth (32). They have concluded the following: (1) the sex difference is due to androgen exposure in utero, (2) androgens promote lung growth, and (3) androgens block both mesenchymal and epithelial maturation.
Our study is limited by its design; because the preterm period of mouse gestation is shorter than that of human pregnancy, it is not possible to use the repetitive doses of GC in intervals recommended for humans. In addition, we did not measure the concentration of BETA and DEX in blood and investigated organs. Caution is necessary when extrapolating from animal models to human clinical medicine, but it is important to point out that the general sequence of growth of organs shows no species differences between laboratory animals and humans. Moreover, it is impossible to conduct a randomized controlled trial of repetitive use of antenatal GC in humans.
Our findings provide experimental support for repetitive treatment courses of antenatal GC for prevention of respiratory distress syndrome in premature infants. However, possible benefits from repetitive dosing must be weighed against increased risks for adverse effects. Exposure to exogenous GC decreases the activity of placental 11β-HSD type 2, which allows increased passage of high maternal GC to the fetus by inhibiting the natural “protective” placental barrier to GC, reduced birth weight, and programmed permanently elevated GC levels throughout the adult life of the newborn (33–36).
We conclude that DEX is less potent than BETA in accelerating fetal lung maturity while causing a greater reduction in fetal LLBW. Repeated administration of GC, especially DEX, should be avoided because of their permanent effect on fetal and neonatal growth. BETA may be preferred in clinical situations requiring imminent preterm labor. In view of these known problems of prolonged GC exposure, retreatment should perhaps be reserved for pregnancies with active labor, recurring more than 1 wk after the last BETA administration, with high risk of delivering an infant at 32 wk gestation. Some aspects of the use of antenatal GC, especially in a repetitive manner, may require reconsideration in humans.
Abbreviations
- SB:
-
single dose of betamethasone
- RB:
-
repetitive doses of betamethasone
- SD:
-
single dose of dexamethasone
- RD:
-
repetitive doses of dexamethasone
- SS:
-
single dose of saline
- RS:
-
repetitive doses of saline
- BETA:
-
betamethasone
- DEX:
-
dexamethasone
- GC:
-
glucocorticoid
- BS:
-
breathing score
- LM:
-
lung maturation
- LLBW:
-
lung, liver and body weights
References
1995 Effect of corticosteroids for fetal maturation on perinatal outcomes. JAMA 273: 413–418
Crowley PA 1995 Antenatal corticosteroid therapy: a meta-analysis of the randomized trials, 1972 to 1994. Am J Obstet Gynecol 173: 322–335
Ikegami M, Polk DH, Jobe AH, Newnham J, Sly P, Kohan R 1996 Effect of interval from corticosteroid treatment to delivery on postnatal lung function in preterm lambs. J Appl Physiol 80: 591–597
Ghidini A, Salafia CM, Minior VK 1977 Repeated courses of steroids in preterm membrane rupture do not increase the risk of histologic chorioamnionitis. Am J Perinatol 14: 309–313
Dirnberger DR, Yoder BA, Gordon MC 2001 Single versus repeated-course antenatal corticosteroids: outcomes in singleton and multiple-gestation pregnancies. Am J Perinatol 18: 267–278
Liley H, White RT, Warr RG, Benson BJ, Hawgood S, Ballard PL 1989 Regulation of messenger RNAs for the hydrophobic surfactant proteins in human lung. J Clin Invest 83: 1191–1197
Modi N, Lewis H, Al-Naqeeb N, Ajayi-Obe M, Dore CJ, Rutherford M 2001 The effects of repeated antenatal glucocorticoid therapy on the developing brain. Pediatr Res 50: 581–585
Bradley BS, Kumar SP, Mehta PN, Ezhuthachan SG 1994 Neonatal cushingoid syndrome resulting from serial courses of antenatal betamethasone. Obstet Gynecol 83: 869–872
Frank L, Roberts RJ 1979 Effects of low-dose prenatal corticosteroid administration on the premature rat. Biol Neonate 36: 1–9
De Souza SW, Adlard BP 1973 Growth of suckling rats after treatment with dexamethasone or cortisol: implications for steroid therapy in human infants. Arch Dis Child 48: 519–522
Barrada MI, Blomquist CH, Kotts C 1980 The effects of betamethasone on fetal development in the rabbit. Am J Obstet Gynecol 136: 234–238
Bloom SL, Sheffield JS, McIntire DD, Leveno KJ 2001 Antenatal dexamethasone and decreased birth weight. Obstet Gynecol 97: 485–490
Rayburn WF, Christensen HD, Gonzalez CL 1997 A placebo-controlled comparison between betamethasone and dexamethasone for fetal maturation: differences in neurobehavioral development of mice offspring. Am J Obstet Gynecol 176: 842–850
Stewart JD, Sienko AE, Gonzalez CL, Christensen HD, Rayburn WF 1998 Placebo-controlled comparison between a single dose and a multidose of betamethasone in accelerating lung maturation of mice offspring. Am J Obstet Gynecol 179: 1241–1247
Christensen H, Sienko A, Rayburn W, Gonzalez C, Coleman F 1996 Selection of a clinically relevant dose of corticosteroids to enhance fetal lung maturity and their effect on fetal growth and development. Teratology 53: 98
Celestone Soluspan suspension 1996 In: Physicians' Desk Reference. 50th ed. Medical Economics, Montvale, NJ, 2130–2131.
Ballard PL, Ballard RA 1995 Scientific basis and therapeutic regimens for use of antenatal glucocorticoids. Am J Obstet Gynecol 173: 254–262
American College of Obstetricians and Gynecologists 1994 Antenatal corticosteroid therapy for fetal maturation. Opinion No. 147. Washington, DC, The College Committee
Stewart JD, Gonzalez CL, Christensen HD, Rayburn WF 1997 Impact of multiple antenatal doses of betamethasone on growth and development of mice offspring. Am J Obstet Gynecol 177: 1138–1144
Ballard PL 2000 Scientific rationale for the use of antenatal glucocorticoids to promote fetal development. Pediatr Rev 1: E83–E90
Seckl JR 1998 Physiologic programming of the fetus. Clin Perinatol 25: 939–962
Celsi G, Kistner A, Aizman R, Eklof AC, Ceccatelli S, de Santiago A, Jacobson SH 1998 Prenatal dexamethasone causes oligonephronia, sodium retention, and higher blood pressure in the offspring. Pediatr Res 44: 317–322
Willet KE, Jobe AH, Ikegami M, Newnham J, Brennan S, Sly PD 2000 Antenatal endotoxin and glucocorticoid effects on lung morphometry in preterm lambs. Pediatr Res 48: 782–788
Corroyer S, Schittny JC, Djonov V, Burri PH, Clement A 2002 Impairment of rat postnatal lung alveolar development by glucocorticoids: involvement of the p21CIP1 and p27KIP1 cyclin-dependent kinase inhibitors. Pediatr Res 51: 169–176
Okajima S, Matsuda T, Cho K, Matsumoto Y, Kobayashi Y, Fujimoto S 2001 Antenatal dexamethasone administration impairs normal postnatal lung growth in rats. Pediatr Res 49: 777–781
Loeb JN 1976 Corticosteroids and growth. N Engl J Med 295: 547–552
Avery ME 1975 Pharmacological approaches to the acceleration of fetal lung maturation. Br Med Bull 31: 13–17
Epstein MF, Farrell PM, Sparks JW, Pepe G, Driscoll SG, Chez RA 1977 Maternal betamethasone and fetal growth and development in the monkey. Am J Obstet Gynecol 127: 261–263
Jobe AH, Polk D, Ikegami M, Newnham J, Sly P, Kohen R, Kelly R 1993 Lung responses to ultrasound-guided fetal treatments with corticosteroids in preterm lambs. J Appl Physiol 75: 2099–2105
Frank L, Roberts RJ 1979 Effects of low-dose prenatal corticosteroid administration on the premature rat. Biol Neonate 36: 1–9
Tabor BL, Rider ED, Ikegami M, Jobe AH, Lewis JF 1991 Dose effects of antenatal corticosteroids for induction of lung maturation in preterm rabbits. Am J Obstet Gynecol 164: 675–681
Torday J 1992 Cellular timing of fetal lung development. Semin Perinatol 16: 130–139
Benediktsson R, Lindsay R, Noble J, Seckl JR, Edwards CRW 1993 Glucocorticoid exposure in utero: a new model for adult hypertension. Lancet 341: 339–341
Lindsay RS, Lindsay RM, Edwards CRW, Seckl JR 1996 Inhibition of 11β-hydroxysteroid dehydrogenase in pregnant rats and the programming of blood pressure in the offspring. Hypertension 27: 1200–1201
Levitt N, Lindsay RS, Holmes MC, Seckl JR 1996 Dexamethasone in the last week of pregnancy attenuates hippocampal glucocorticoid receptor gene expression and elevates blood pressure in the adult offspring in the rat. Neuroendocrinology 64: 412–418
Benediktsson R, Calder AA, Edwards CRW, Seckl JR 1997 Placental 11β-hydroxysteroid dehydrogenase type 2 is the placental barrier to maternal glucocorticoids: ex vivo studies. Clin Endocrinol 46: 161–166
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ozdemir, H., Guvenal, T., Cetin, M. et al. A Placebo-Controlled Comparison of Effects of Repetitive Doses of Betamethasone and Dexamethasone on Lung Maturation and Lung, Liver, and Body Weights of Mouse Pups. Pediatr Res 53, 98–103 (2003). https://doi.org/10.1203/00006450-200301000-00017
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-200301000-00017
This article is cited by
-
Prenatal glucocorticoid administration accelerates the maturation of fetal rat hepatocytes
Molecular Biology Reports (2022)
-
Effects of antenatal betamethasone on preterm human and mouse ductus arteriosus: comparison with baboon data
Pediatric Research (2018)
-
Transgenically-expressed secretoglobin 3A2 accelerates resolution of bleomycin-induced pulmonary fibrosis in mice
BMC Pulmonary Medicine (2015)