Abstract
Introduction
Insulin degludec (degludec), an ultra-long-acting basal insulin analogue, provides equivalent glycemic control to other basal insulin analogues, with lower risk of hypoglycemia and flexible dosing. Chinese TREsiba AudiT (CN-TREAT) investigated outcomes with degludec in people with type 2 diabetes (T2D) in routine clinical practice in China.
Methods
This was a retrospective chart review study in adults with T2D initiating or switching to degludec at 50 sites in China between January 2020 and July 2021. The primary endpoint was change in glycated hemoglobin (HbA1c) from baseline to end of study (EOS; week 20). Secondary endpoints included change from baseline to EOS in fasting plasma glucose (FPG), self-measured plasma glucose (SMPG), daily insulin dose, and rate of hypoglycemia.
Results
Data from 936 participants were included (499 insulin-naïve; 437 insulin-experienced). Mean (95% confidence interval [CI]) HbA1c change from baseline to EOS was − 1.48%-points (− 1.57; − 1.38; P < 0.0001) overall: − 1.95%-points (− 2.08; − 1.81; P < 0.0001) in insulin-naïve participants and − 0.95%-points (− 1.08; − 0.82; P < 0.0001) in insulin-experienced participants. Mean (95% CI) changes in FPG and SMPG were − 2.27 mmol/L (− 2.69; − 1.85; P < 0.0001) and − 2.89 mmol/L (− 3.52; − 2.25; P < 0.0001), respectively, with similar reductions in insulin-naïve and insulin-experienced subgroups. Rate of hypoglycemia did not change statistically significantly from baseline to EOS overall, or in insulin-experienced participants, except when adjusted for baseline hypoglycemia. Basal insulin dose did not change statistically significantly in insulin-experienced participants.
Conclusion
In routine clinical practice in China, initiation or switching to degludec was associated with improvements in glycemic control in people with T2D, with no increased risk of hypoglycemia.
Trial Registration
ClinialTrials.gov, NCT04227431.
Similar content being viewed by others
Why carry out this study? |
Insulin degludec (degludec) is an ultra-long-acting insulin analogue that has been found to have clinical benefits in randomized controlled trials and, more recently, in real-world observational studies in people with type 1 diabetes or type 2 diabetes (T2D). |
Until now, however, degludec had not been studied in a real-world setting in a Chinese population, so this study aimed to assess glycemic control and risk of hypoglycemia following initiation or switching to degludec in adults with T2D in real-world clinical practice in China. |
What was learned from the study? |
There were improvements in glycemic control in the total population (− 1.48%-point HbA1c change; P < 0.0001), and in subgroups of insulin-naïve (− 1.95%-point change; P < 0.0001) and insulin-experienced (− 0.95%-point change; P < 0.0001) participants over the 20-week study period, without the risk of hypoglycemia increasing overall or in insulin-experienced participants. |
In routine clinical practice in China, initiation or switching to degludec was associated with improvements in glycemic control in people with T2D, with no increased risk of hypoglycemia, consistent with findings from studies of other populations. |
Introduction
Insulin degludec (degludec) is an ultra-long-acting basal insulin analogue with a half-life of approximately 25 h and a duration of action at steady state greater than 42 h, exceeding its once-daily dosing interval [1,2,3,4,5,6]. This results in a very stable pharmacokinetic/pharmacodynamic profile that more closely mimics the physiological insulin profile, translating clinically into low within-day and day-to-day variability in blood glucose-lowering effect, compared with insulin glargine 100 units/mL (glargine U100) or insulin glargine 300 units/mL (glargine U300) [1,2,3,4,5,6]. The stable, protracted profile of degludec also enables flexible dosing, once daily at any time of the day, but preferably at the same time, with a minimum of 8 h between doses [6, 7].
Randomized controlled trials (RCTs) in people with type 1 diabetes (T1D) or type 2 diabetes (T2D) have demonstrated equivalent levels of glycemic control with degludec compared to other basal insulin analogues, particularly glargine U100, accompanied by a reduced risk of hypoglycemia [8,9,10,11,12,13]. RCTs in people with T2D have been carried out in insulin-naïve participants initiating degludec [14,15,16,17,18,19,20,21] and in insulin-experienced participants switching from another basal insulin to degludec [22, 23]. Furthermore, results from a large, randomized cardiovascular outcomes trial (DEVOTE) demonstrated that degludec was non-inferior to glargine U100 with respect to the incidence of major cardiovascular events in people with T2D at high risk for cardiovascular events [24].
Degludec was approved in China for the treatment of adults with T2D in 2017 [25] following results from a multinational, randomized, open-label, treat-to-target trial in insulin-naïve people with T2D (with a majority of Chinese participants) [16]. Results demonstrated a numerically lower risk for overall and nocturnal hypoglycemia with degludec than with glargine U100, with similar levels of glycemic control [16].
In addition to the data generated from RCTs, it is important to collect supporting data on the use of degludec in a real-world clinical setting. RCTs can be limited by their study design and inclusion criteria, and may not accurately reflect routine clinical practice [26].
Several prospective, observational, single-arm studies in people with T1D at a single center [27], and in people with T1D or T2D in Europe [28], reported improved glycemic control and reduced risk of hypoglycemia after switching to degludec from other basal insulins. Similar results were also seen in a single-center retrospective case series analysis in people with T1D or T2D [29]. Larger retrospective, multicenter, non-interventional chart review studies, in people with T1D or T2D switching to degludec from other basal insulins in routine clinical practice, have been carried out both in Europe and in Canada. The European EU-TREAT study demonstrated improved glycemic control and a statistically significantly reduced risk of hypoglycemia after switching to degludec [30], while the Canadian CAN-TREAT study demonstrated improved glycemic control, with either improvement or no change in hypoglycemia rates on switching to degludec [31].
The current study (Chinese TREsiba AudiT [CN-TREAT]) is the first to assess glycemic control and risk of hypoglycemia following initiation or switching to degludec in adults with T2D in real-world clinical practice in China.
Methods
Study Design
This was a non-interventional, retrospective chart review study (NCT04227431), collecting data reported in the medical records of people with T2D who initiated degludec (adding it to existing non-insulin antidiabetic drug treatment) or switched to degludec from another basal insulin (± non-insulin antidiabetic drugs, ± prandial insulin) and who were treated for at least 20 weeks. The study collected data from routine clinical practice at 50 sites across China in the period from January 17, 2020 to July 17, 2021. All 50 sites were public hospitals located in urban regions. Key considerations in site selection were availability and consumption of degludec, investigator interest in the study, quality of records, and past collaboration experience. The study design is summarized in Fig. 1.
Study design. Data from 20 weeks prior to degludec initiation to the EOS were extracted anonymously from medical records and entered into a secure EDC registry database via eCRF. Baseline was defined as a period of ≤ 12 weeks prior to degludec initiation (week 0). EOS was defined as 20 ± 8 weeks after degludec initiation. If multiple values were available for the specific endpoints, the value closest to week 20 was used. Degludec insulin degludec, eCRF electronic case report form, EDC electronic data capture, EOS end of study, OAD oral antidiabetic drug
Eligible individuals were aged ≥ 18 years, diagnosed with T2D, and treated with any non-insulin antidiabetic drugs or basal insulin ± non-insulin antidiabetic drugs, ± prandial insulin, for at least 20 weeks prior to treatment initiation with degludec. They were treated with degludec (± non-insulin antidiabetic drugs, ± prandial insulin) in accordance with the local label for at least 20 weeks, and had an available HbA1c value within 12 weeks prior to degludec initiation and in the first 20 weeks (± 8 weeks) after degludec initiation. Exclusion criteria included participation in a diabetes clinical trial (of any approved or non-approved medicinal product) within 20 weeks prior to degludec initiation, or during the first 28 weeks of treatment with degludec, and use of continuous subcutaneous insulin infusion or premix insulin (for > 14 days) within 20 weeks prior to degludec initiation. The decision to initiate degludec was made by the individual/legally acceptable representative and the treating physician before and independently from the decision to include the individual’s data in this study. Relevant data for eligible participants were abstracted anonymously from their medical records and entered by study sites into a secure internet-based electronic data capture (EDC) registry database via electronic case report form (eCRF), after their signed informed consent had been given. Appropriate measures such as encryption or deletion were enforced to protect the identity of study participants when transmitting data.
Ethical Approval
The study was conducted in accordance with the Declaration of Helsinki [32] and the Guidelines for Good Pharmacoepidemiology Practices [33]. Informed consent was obtained from each participant, granting permission to obtain and process the medical record data needed to complete the study. Prior to study initiation, the protocol, any amendments, participant information/informed consent form (ICF), any other written information to be provided to the participant, and participant enrolment procedures were reviewed and approved by an independent ethics committee (IEC)/institutional review board (IRB) (or other appropriate bodies as required locally). A list of the IECs/IRBs that reviewed and approved the protocol, including approval dates, is provided in the Supplementary Appendix.
Study Endpoints
The primary endpoint was change in HbA1c (%-points) from baseline to end of study (EOS). Secondary endpoints included change in laboratory-measured fasting plasma glucose (FPG), self-measured plasma glucose (SMPG), or daily insulin dose (total, basal, and prandial) from baseline to EOS, change in rates of hypoglycemic episodes (number of episodes/person-years) (overall, severe) before and after degludec initiation, change in number of concomitant non-insulin antidiabetic drugs before and after degludec initiation, and reason(s) for starting degludec, at time of initiation, if available.
For the purposes of data collection, EOS was defined as 20 weeks after degludec initiation, with a window of ± 8 weeks. If multiple values were available for specific endpoints, the value closest to week 20 was used. Baseline was defined as a timepoint ≤ 12 weeks prior to degludec initiation. Hypoglycemic episodes were collected within 20 weeks before and after degludec initiation. Severe hypoglycemia was defined as an episode that required assistance from another person to actively administer carbohydrate, glucagon, or other corrective actions. All data were recorded on the basis of information available in the patient medical records. Clear definitions of all study variables and detailed eCRF instructions were provided, and eCRF data entry was completed by trained individuals. The eCRF included programmable edit checks to identify missing, out of range, illogical, or potentially erroneous data, and routine monitoring and source data verification were performed. As a retrospective chart review study, no safety reporting was included.
Statistical Methods
The study sample size was calculated to have sufficient power for the primary endpoint analysis in the insulin-naïve and insulin-experienced subgroups defined below, based on the following assumptions: an even distribution of participants from each treatment regimen at baseline; a mean decrease of 0.3%-points in HbA1c considered as a clinically relevant change; the standard deviation (SD) of the change in HbA1c assumed to be 2.0%-points; and an overall power level of 90%.
On the basis of these assumptions, a minimum of 469 individuals were required in each subgroup, i.e., a total of 938 participants in the study. Analyses were carried out on the full analysis set (FAS), defined as all participants who signed informed consent and met the eligibility criteria, with two subgroups defined: the insulin-naïve analysis set—individuals who were treated with non-insulin antidiabetic drugs prior to treatment degludec initiation; and the insulin-experienced analysis set—individuals who were treated with basal insulin (± non-insulin antidiabetic drugs, ± prandial insulin) prior to degludec initiation, and who had their basal insulin switched to degludec.
The primary endpoint (change from baseline to EOS in HbA1c) was analyzed using an analysis of covariance (ANCOVA) model, with baseline HbA1c, age, gender (male or female), and duration of diabetes (< 5, 5–10, 10–15, or 15+ years) as covariates. Change from baseline to EOS in FPG, SMPG, and daily insulin dose were also analyzed using an ANCOVA model with baseline measurement, age, gender (male or female), and duration of diabetes (< 5, 5–10, 10–15, or 15+ years) as covariates. Change in rate of hypoglycemic episodes and in concomitant non-insulin antidiabetic drugs before and after degludec initiation were analyzed using a negative binomial model with baseline measurement, age, gender (male or female), and duration of diabetes (< 5, 5–10, 10–15, or 15+ years) as covariates.
In general, missing data were not imputed (except for dates), and the data were analyzed as recorded in the study eCRFs. If only day of start date was missing, it was imputed to the first day of that month. If only day of stop date was missing, it was imputed to the last day of the month, death date, or date of withdrawal, whichever was earlier. If either the month or the year elements of the event date were missing, the date was not imputed and was assigned a missing value.
Results
Study Population Demographics and Clinical Characteristics
A total of 1116 individuals were screened and, of these, data from 936 were included in the FAS (499 insulin-naïve, 437 insulin-experienced). Baseline characteristics are summarized in Table 1. All participants in the insulin-experienced subgroup had received at least one basal insulin therapy prior to degludec initiation, the most frequently reported being insulin glargine (n = 427, 66.4%). The mean (SD) duration of treatment for participants with at least one basal insulin therapy was 2.1 (2.96) years. At least one prandial insulin had been used by 41.6% (n = 182) of participants in the insulin-experienced subgroup prior to degludec initiation. The most commonly used non-insulin antidiabetic drugs in both subgroups were metformin and alpha-glucosidase inhibitors. The reasons given for switching to degludec are also presented in Table 1. In both subgroups, the need to improve glycemic control was the most frequently given reason (61.1% of participants), followed by the desire to reduce blood glucose fluctuations (28.3%). By EOS, 5.2% of participants had discontinued degludec, with treatment ongoing for 94.8% (n = 887) of the total population, (95% [n = 474] of the insulin-naïve subgroup, and 94.5% [n = 413] of the insulin-experienced subgroup).
Glycemic Control
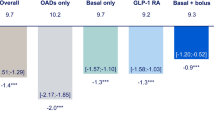
Mean (SD) HbA1c values at baseline and EOS were 9.38% (2.12) and 7.86% (1.60), respectively, in the total population; 9.66% (2.10) and 7.65% (1.54), respectively, in the insulin-naïve subgroup; and 9.05% (2.10) and 8.11% (1.63), respectively, in the insulin-experienced subgroup. Following adjustment for covariates, the least squares (LS) mean (95% confidence interval [CI]) change from baseline to EOS in HbA1c was − 1.48%-points (− 1.57; − 1.38; P < 0.0001) in the total population, with corresponding reductions in insulin-naïve and insulin-experienced subgroups of − 1.95%-points (− 2.08; − 1.81; P < 0.0001) and − 0.95%-points (− 1.08; − 0.82; P < 0.0001), respectively (Fig. 2). Statistically significant reductions in HbA1c were observed from baseline to EOS for all covariates and their categories, except for age (Supplementary Table S1).
Change in HbA1c from baseline to EOS. Analysis was by ANCOVA, with baseline HbA1c, age, gender (male or female), and duration of diabetes (< 5, 5–10, 10–15, or > 15 years) as covariates. For duration of diabetes, due to limited number of patients, the categories “< 1 year” and “1–5 years” were combined in “< 5 years”. Baseline was defined as a period of ≤ 12 weeks prior to degludec initiation. EOS was defined as 20 ± 8 weeks after degludec initiation. ANCOVA analysis of covariance, CI confidence interval, EOS end of study, HbA1c glycated hemoglobin, LS least squares
Data for FPG and SMPG were unavailable for the majority of patients, but the available observed data are summarized in Table 2. Following adjustment for covariates, the LS mean (95% CI) change in FPG from baseline to EOS was − 2.27 mmol/L (− 2.69; − 1.85; P < 0.0001) in the total population, with corresponding reductions in insulin-naïve and insulin-experienced subgroups of − 3.22 mmol/L (− 3.77; − 2.68; P < 0.0001) and − 0.86 mmol/L (− 1.57; − 0.15; P = 0.0176), respectively.
Following adjustment for covariates, the LS mean (95% CI) change from baseline to EOS in SMPG was − 2.89 mmol/L (− 3.52; − 2.25; P < 0.0001) in the total population, with corresponding reductions in insulin-naïve and insulin-experienced subgroups of − 2.76 mmol/L (− 3.88; − 1.64; P < 0.0001) and − 3.00 mmol/L (− 3.70; − 2.29; P < 0.0001), respectively.
Insulin Dose
Descriptive statistics for observed daily insulin dose are presented in Table 2. Following adjustment for covariates, in insulin-experienced participants, the mean (95% CI) change from baseline to EOS in basal insulin dose was not statistically significant (− 0.26 units/day [− 0.82; 0.29; P = 0.354]). However, small but statistically significant mean (95% CI) decreases were seen from baseline to EOS in prandial insulin dose (− 3.86 units/day [− 5.66; − 2.07]; P < 0.0001) and total insulin dose (− 1.52 units/day [− 2.08; − 0.97]; P < 0.0001).
Hypoglycemia
A summary of data for hypoglycemia is presented in Table 3. The event rates were low and differed little between baseline and EOS. Only a small proportion of the total population experienced severe hypoglycemia, equating to a rate of 0.03 (95% CI 0.01; 0.05) episodes per person-year at baseline and 0.02 (95% CI 0.01; 0.04) episodes per person-year at EOS.
In the total population, the hypoglycemic episodes rate at EOS was not statistically significantly different from that at baseline, following adjustment for covariates, except for baseline hypoglycemic episodes (incidence rate ratio, IRR 1.22 [95% CI 1.03; 1.46] in univariate analysis; IRR 1.22 [95% CI 1.02; 1.47] in multivariate analysis) (Supplementary Table S2). In the insulin-experienced subgroup, the rate of hypoglycemic episodes at EOS was also only statistically significantly different from that at baseline following adjustment for baseline hypoglycemic episodes (IRR 1.46 [95% CI 1.08; 1.96] in univariate analysis; IRR 1.44 [95% CI 1.05; 1.99] in multivariate analysis). In the insulin-naïve subgroup, the rate of hypoglycemic episodes at EOS was only statistically significantly different to baseline following adjustment for duration of diabetes (for the category of 5–10 years, compared to a reference value of < 5 years; IRR 13.43 [95% CI 2.98; 60.51]; univariate analysis).
Concomitant Non-insulin Antidiabetic Drugs
In the total population, the mean (SD) number of non-insulin antidiabetic drugs was 2.6 (1.47) at baseline (n = 866) and 2.2 (1.68) at EOS (n = 572). The respective numbers were 2.8 (1.63) and 2.3 (1.68) in the insulin-naïve subgroup, and 2.3 (1.19) and 2.2 (1.67) in the insulin-experienced subgroup. The mean (SD) change from baseline to EOS in number of non-insulin antidiabetic drugs was − 0.4 (2.00) in the total population, − 0.5 (2.04) in the insulin-naïve subgroup, and − 0.2 (1.92) in the insulin-experienced subgroup (Supplementary Table S3). By negative binomial analysis, baseline non-insulin antidiabetic drugs, age, and gender were statistically significant determinants of this change in the number of concomitant non-insulin antidiabetic drugs from baseline to EOS (Supplementary Table S4).
Discussion
This real-world, retrospective chart review study found that use of degludec in people in China with T2D was associated with lower levels of HbA1c in both insulin-naïve and insulin-experienced individuals. This was accompanied by lower FPG and SMPG in both subgroups. For FPG, the decrease seen from baseline to EOS was greater in the insulin-naïve group, whereas, for SMPG, there was a greater decrease in the insulin-experienced group. However, this apparent discrepancy should be viewed with caution due to a high proportion of missing data for these secondary endpoints.
Importantly, these clinically valuable decreases in HbA1c and fasting glucose values did not come at the cost of an increased risk of hypoglycemia. While there was a statistically significantly higher number of hypoglycemic events following treatment, the overall risk of hypoglycemic events remained low. Only small numbers of insulin-naïve participants experienced episodes of severe and non-severe hypoglycemia at baseline, and these increased only slightly after the initiation of insulin. In the insulin-experienced subgroup, the proportions of individuals with severe and non-severe hypoglycemia at baseline changed little despite the improved HbA1c. Additionally, improved glycemic control was achieved with little change in insulin dose in insulin-experienced participants, and a small reduction in the number of non-insulin antidiabetic drugs in both subgroups. Degludec has a well-documented, relatively low risk of hypoglycemia compared with other basal insulin analogues [9, 10, 13, 22], yet the need to avoid hypoglycemia was not a common reason for its initiation in this study. The main reason for switching to degludec was to reduce hyperglycemia, and the data suggest that it was successful in this regard. Interestingly, the need to reduce blood glucose fluctuations was also cited as a common reason for initiating degludec.
CN-TREAT was a large-scale, multicenter study and the first to investigate treatment with degludec in people with T2D in a real-world setting in China. The range of T2D duration among participants was large (from < 1 to > 15 years). While outside the scope of this study, an interesting focus of a future study would be to investigate the effectiveness of initiating or switching to degludec in participants with different disease durations in real clinical practice. No missing data were reported for the results for the primary endpoint, change in HbA1c from baseline to EOS. The results presented here are in alignment with those from the T2D cohorts of the EU-TREAT [30] and CAN-TREAT [31] studies, in which insulin-experienced individuals switching to degludec from other basal insulins were studied using similar methodology to ours. These studies also demonstrated improvements in HbA1c with degludec, with no concomitant increase in insulin dose or hypoglycemia risk. The mean change in HbA1c from baseline to EOS was − 0.51%-points in EU-TREAT [30] and − 0.4%-points in CAN-TREAT [31]. The decline in FPG values from baseline to EOS reported in this study was also in line with the decrease in FPG reported in the EU-TREAT and CAN-TREAT studies, which both reported mean reductions of − 1.31 mmol/L 6 months after switching to degludec [30, 31].
The baseline HbA1c values for participants of CN-TREAT were notably higher (9.66% for the insulin-naïve subgroup; 9.05% for the insulin-experienced subgroup) than those for the T2D cohort of EU-TREAT (8.4%) [30] or CAN-TREAT (8.3%) [31]. This may indicate late initiation or suboptimal titration of basal insulin in real-world clinical practice in China, and emphasizes a need for more timely initiation or switching to degludec in this population, and the importance of adequate insulin dose titration to optimize glycemic control.
Limitations
There are some potential limitations that should be considered when interpreting this study. As this was a non-interventional, retrospective study, bias and potential confounding factors cannot be ruled out. Although broad eligibility criteria were selected to minimize selection bias, this was still a possibility, since the sites were selected with consideration of the availability of degludec, investigator interest in the study, quality of records, and past collaboration experience. In addition, bias could have resulted from potential treatment discontinuation in participants not achieving clinical success or with poor access to medication, and possibly because of recruitment only from urban areas. Although efforts were made to minimize information bias, there was no control over how data were recorded or managed, nor the accuracy of the assessment of study variables. Originally, the statistical calculations suggested that a minimum of 469 individuals were required in each subgroup for the study to be sufficiently powered. However, in the final analysis, only 437 participants were included in the insulin-experienced population. While this likely did not impact the overall conclusions of the study, and to some extent reflects real-world treatment patterns, this small shortfall should be acknowledged. Hypoglycemic episodes, particularly those that are non-severe, may be underreported in these types of study, and there may also be a bias for reporting episodes post-degludec initiation when participants are being more closely observed, especially if they are insulin-naïve. A limitation of the data collected for SMPG is that values were a combination of assessments with either fasting, non-fasting, or unknown status of the patient. In addition, a large proportion of participants did not have data for FPG and SMPG, making interpretation of the ANCOVA models less reliable. Missing data may be an issue in real-world studies if there is limited control over data collection [34], and, as a result of SMPG data being collected by the patient, there was little control over sampling technique and timing. Analyses of change in daily insulin doses and change in number of concomitant non-insulin antidiabetic drugs were also limited by the way data were collected. Approximately 15–20% of medication records for basal, prandial insulin, and non-insulin antidiabetics were based on durations as a result of start and end dates not being available. It is also worth noting that only associations between treatment and outcomes, rather than causal relationships, can be derived from studies of this type. Finally, as the COVID-19 pandemic started in early 2020, part of the population was treated during the pandemic, which may have impacted upon standard of care and data collection.
Conclusions
Treatment of insulin-naïve or insulin-experienced people with T2D with degludec in real-world clinical practice in China was associated with improved glycemic control. In insulin-experienced individuals, this was achieved with no statistically significant increase in daily basal insulin dose and no statistically significant change in the rate of hypoglycemia. These findings are in alignment with other large real-world evidence studies of similar design and suggest that degludec may be a favorable option for the management of people with T2D with suboptimal glycemic control on their current treatment.
Data Availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Heise T, Hermanski L, Nosek L, Feldman A, Rasmussen S, Haahr H. Insulin degludec: four times lower pharmacodynamic variability than insulin glargine under steady-state conditions in type 1 diabetes. Diabetes Obes Metab. 2012;14:859–64.
Heise T, Nosek L, Bøttcher SG, Hastrup H, Haahr H. Ultra-long-acting insulin degludec has a flat and stable glucose-lowering effect in type 2 diabetes. Diabetes Obes Metab. 2012;14:944–50.
Heise T, Nørskov M, Nosek L, Kaplan K, Famulla S, Haahr HL. Insulin degludec: lower day-to-day and within-day variability in pharmacodynamic response compared with insulin glargine 300 U/mL in type 1 diabetes. Diabetes Obes Metab. 2017;19:1032–9.
Jonassen I, Havelund S, Hoeg-Jensen T, Steensgaard DB, Wahlund PO, Ribel U. Design of the novel protraction mechanism of insulin degludec, an ultra-long-acting basal insulin. Pharm Res. 2012;29:2104–14.
Ooi CP, Ting TH, Lye MS. Ultra-long acting insulin versus long-acting insulin for type 1 diabetes mellitus. Cochrane Database Syst Rev. 2018;2018(7):CD011102. https://doi.org/10.1002/14651858.CD011102.pub2.
Novo Nordisk. IDeg®. Summary of Product Characteristics. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/002498/WC500138940.pdf. Accessed Oct 28, 2022.
Josse RG, Woo V. Flexibly timed once-daily dosing with degludec: a new ultra-long-acting basal insulin. Diabetes Obes Metab. 2013;15:1077–84.
Davies M, Sasaki T, Gross JL, et al. Comparison of insulin degludec with insulin detemir in type 1 diabetes: a 1-year treat-to-target trial. Diabetes Obes Metab. 2016;18:96–9.
Lane W, Bailey TS, Gerety G, et al. Effect of insulin degludec vs insulin glargine U100 on hypoglycemia in patients with type 1 diabetes: the SWITCH 1 randomized clinical trial. JAMA. 2017;318:33–44.
Ratner RE, Gough SC, Mathieu C, et al. Hypoglycaemia risk with insulin degludec compared with insulin glargine in type 2 and type 1 diabetes: a pre-planned meta-analysis of phase 3 trials. Diabetes Obes Metab. 2013;15:175–84.
Vora J, Cariou B, Evans M, et al. Clinical use of insulin degludec. Diabetes Res Clin Pract. 2015;109:19–31.
Vora J, Christensen T, Rana A, Bain SC. Insulin degludec versus insulin glargine in type 1 and type 2 diabetes mellitus: a meta-analysis of endpoints in phase 3a trials. Diabetes Ther. 2014;5:435–46.
Zhou W, Tao J, Zhou X, Chen H. Insulin degludec, a novel ultra-long-acting basal insulin versus insulin glargine for the management of type 2 diabetes: a systematic review and meta-analysis. Diabetes Ther. 2019;10:835–52.
Aso Y, Suzuki K, Chiba Y, et al. Effect of insulin degludec versus insulin glargine on glycemic control and daily fasting blood glucose variability in insulin-naïve Japanese patients with type 2 diabetes: I’D GOT trial. Diabetes Res Clin Pract. 2017;130:237–43.
Rosenstock J, Cheng A, Ritzel R, et al. More similarities than differences testing insulin glargine 300 units/mL versus insulin degludec 100 units/mL in insulin-naive type 2 diabetes: the randomized head-to-head BRIGHT trial. Diabetes Care. 2018;41:2147–54.
Pan C, Gross JL, Yang W, et al. A multinational, randomized, open-label, treat-to-target trial comparing insulin degludec and insulin glargine in insulin-naïve patients with type 2 diabetes mellitus. Drugs R D. 2016;16:239–49.
Onishi Y, Iwamoto Y, Yoo SJ, Clauson P, Tamer SC, Park S. Insulin degludec compared with insulin glargine in insulin-naïve patients with type 2 diabetes: a 26-week, randomized, controlled, Pan-Asian, treat-to-target trial. J Diabetes Investig. 2013;4:605–12.
Zinman B, DeVries JH, Bode B, et al. Efficacy and safety of insulin degludec three times a week versus insulin glargine once a day in insulin-naive patients with type 2 diabetes: results of two phase 3, 26 week, randomised, open-label, treat-to-target, non-inferiority trials. Lancet Diabetes Endocrinol. 2013;1:123–31.
Rodbard HW, Cariou B, Zinman B, et al. Comparison of insulin degludec with insulin glargine in insulin-naive subjects with type 2 diabetes: a 2-year randomized, treat-to-target trial. Diabet Med. 2013;30:1298–304.
Gough SC, Bhargava A, Jain R, Mersebach H, Rasmussen S, Bergenstal RM. Low-volume insulin degludec 200 units/ml once daily improves glycemic control similarly to insulin glargine with a low risk of hypoglycemia in insulin-naive patients with type 2 diabetes: a 26-week, randomized, controlled, multinational, treat-to-target trial: the BEGIN LOW VOLUME trial. Diabetes Care. 2013;36:2536–42.
Zinman B, Philis-Tsimikas A, Cariou B, et al. Insulin degludec versus insulin glargine in insulin-naive patients with type 2 diabetes: a 1-year, randomized, treat-to-target trial (BEGIN Once Long). Diabetes Care. 2012;35:2464–71.
Wysham C, Bhargava A, Chaykin L, et al. Effect of insulin degludec vs insulin glargine U100 on hypoglycemia in patients with type 2 diabetes: the SWITCH 2 randomized clinical trial. JAMA. 2017;318:45–56.
Hollander P, King AB, Del Prato S, et al. Insulin degludec improves long-term glycaemic control similarly to insulin glargine but with fewer hypoglycaemic episodes in patients with advanced type 2 diabetes on basal-bolus insulin therapy. Diabetes Obes Metab. 2015;17:202–6.
Marso SP, McGuire DK, Zinman B, et al. Efficacy and safety of degludec versus glargine in type 2 diabetes. N Engl J Med. 2017;377:723–32.
Novo Nordisk. Tresiba® package insert (Insulin Degludec Injection). National Medical Products Administration. https://www.nmpa.gov.cn/datasearch/search-info.html?nmpa=aWQ9MTI5ZTY2YWM4ZTY0ODBjODYyY2VlNTVhMDRhNzFlOGYmaXRlbUlkPWZmODA4MDgxODNjYWQ3NTAwMTg0MDg4NjY1NzExODAw. Accessed Jan 04, 2023.
Blonde L, Khunti K, Harris SB, Meizinger C, Skolnik NS. Interpretation and impact of real-world clinical data for the practicing clinician. Adv Ther. 2018;35:1763–74.
Landstedt-Hallin L. Changes in HbA1c, insulin dose and incidence of hypoglycemia in patients with type 1 diabetes after switching to insulin degludec in an outpatient setting: an observational study. Curr Med Res Opin. 2015;31:1487–93.
Fadini GP, Feher M, Hansen TK, et al. Switching to degludec from other basal insulins is associated with reduced hypoglycemia rates: a prospective study. J Clin Endocrinol Metab. 2019;104:5977–90.
Evans M, McEwan P, Foos V. Insulin degludec early clinical experience: does the promise from the clinical trials translate into clinical practice—a case-based evaluation. J Med Econ. 2015;18:96–105.
Siegmund T, Tentolouris N, Knudsen ST, et al. A European, multicentre, retrospective, non-interventional study (EU-TREAT) of the effectiveness of insulin degludec after switching basal insulin in a population with type 1 or type 2 diabetes. Diabetes Obes Metab. 2018;20:689–97.
Harris SB, Ajala O, Bari B, et al. Evaluating the effectiveness of switching to insulin degludec from other basal insulins in a real-world Canadian population with type 1 or type 2 diabetes: the CAN-TREAT study. Diabetes Ther. 2021;12:1689–702.
World Medical Association. The WMA's Declaration of Helsinki on Ethical Principles for Medical Research Involving Human Subjects. 2008. https://www.wma.net/policies-post/wma-declaration-of-helsinki-ethical-principles-for-medical-research-involving-human-subjects/. Accessed Nov 02, 2022.
International Society for Pharmacoepidemiology. Guidelines for Good Pharmacoepidemiology Practices. 2007. https://www.pharmacoepi.org/resources/policies/guidelines-08027/. Accessed Oct 28, 2022.
Gueyffier F, Cucherat M. The limitations of observation studies for decision making regarding drugs efficacy and safety. Therapie. 2019;74:181–5.
Acknowledgements
We thank the participants for their involvement in the study.
Medical Writing and Editorial Assistance
Medical writing and editorial support for the development of this manuscript, under the direction of the authors, were provided by Carrie Fielden, MSc, Jane Blackburn, PhD, Sherriden Beard, MA, and Helen Marshall, BA, of Ashfield MedComms, an Inizio company, and funded by Novo Nordisk.
Funding
The study and the journal’s Rapid Service Fee were funded by Novo Nordisk.
Author information
Authors and Affiliations
Contributions
Mads Nordentoft contributed to study design, data collection, data analysis, and data interpretation. Weimin Wang, Xiangyun Chang, Lars Lang Lehrskov, Ling Li, Mads Nordentoft, Jinxing Quan, Yubo Sha, Xing Zhong, Caixian Yang, and Dalong Zhu contributed to critical review and revision of the manuscript, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published. All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship of this article.
Corresponding author
Ethics declarations
Conflict of Interest
Weimin Wang, Xiangyun Chang, Ling Li, Jinxing Quan, Yubo Sha, Caixian Yang, and Dalong Zhu declare that they have no competing interests. Mads Nordentoft is an employee of, and also holds shares in, Novo Nordisk A/S. Lars Lang Lehrskov was an employee of and held shares in Novo Nordisk A/S at the time of the study completion. Lars no longer works for Novo Nordisk; current affiliation is Kirurg hos Kirurgisk Klinik, Allerød, Denmark. Xing Zhong is an employee of, and also holds shares in, Novo Nordisk (Shanghai) Pharma Trading Co, Ltd.
Ethical Approval
The study was conducted in accordance with the Declaration of Helsinki [32] and the Guidelines for Good Pharmacoepidemiology Practices [33]. Informed consent was obtained from each participant, granting permission to obtain and process the medical record data needed to complete the study. Prior to study initiation, the protocol, any amendments, patient information/informed consent form (ICF), any other written information to be provided to the patient, and patient enrolment procedures were reviewed and approved by an independent ethics committee (IEC)/institutional review board (IRB) (or other appropriate bodies as required locally). A list of the IECs/IRBs that reviewed and approved the protocol, including approval dates, is provided in the Supplementary Appendix.
Additional information
Prior Publication: Results from this study have previously been presented in poster form at IDF 2022 (Zhu D et al. poster presented at the International Diabetes Federation congress, 5–8 December 2022, Lisbon, Portugal [poster number LI2022-0438]); accepted abstract available at https://www.diabetesresearchclinicalpractice.com/article/S0168-8227(23)00288-7/fulltext).
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Wang, W., Chang, X., Lehrskov, L.L. et al. Insulin Degludec in People with Type 2 Diabetes in China: A Non-interventional, Retrospective Chart Review Study (CN-TREAT). Diabetes Ther 15, 725–739 (2024). https://doi.org/10.1007/s13300-024-01533-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13300-024-01533-6